In my work with clients who are survivors of trauma, I’m frequently asked the differences and similarities between PTSD (post traumatic stress disorder) and complex PTSD as well as where BPD (borderline personality disorder) fits into the diagnoses and if it’s connected. Let’s break it all down to get a better understanding and why it even matters.
The first thing we need to look at are two separate, though oftentimes intertwined classification systems, the DSM-5-TR and the ICD-11. The DSM-5-TR (The Diagnostic and Statistical Manual of Mental Disorder, 5th edition, Text Revision) was updated in 2022 by the APA (American Psychiatric Association), mostly for clarity and for the addition of a new diagnosis pertaining to prolonged grief as well as for symptom codes for reporting suicidal and nonsuicidal self harm. The DSM-5-TR is primarily used in North America. In contrast, the ICD-11 (the International Classification of Diseases, 11th edition) is a worldwide classification system not only for mental illnesses, but also for physical illnesses and is published by the World Health Organization (WHO).
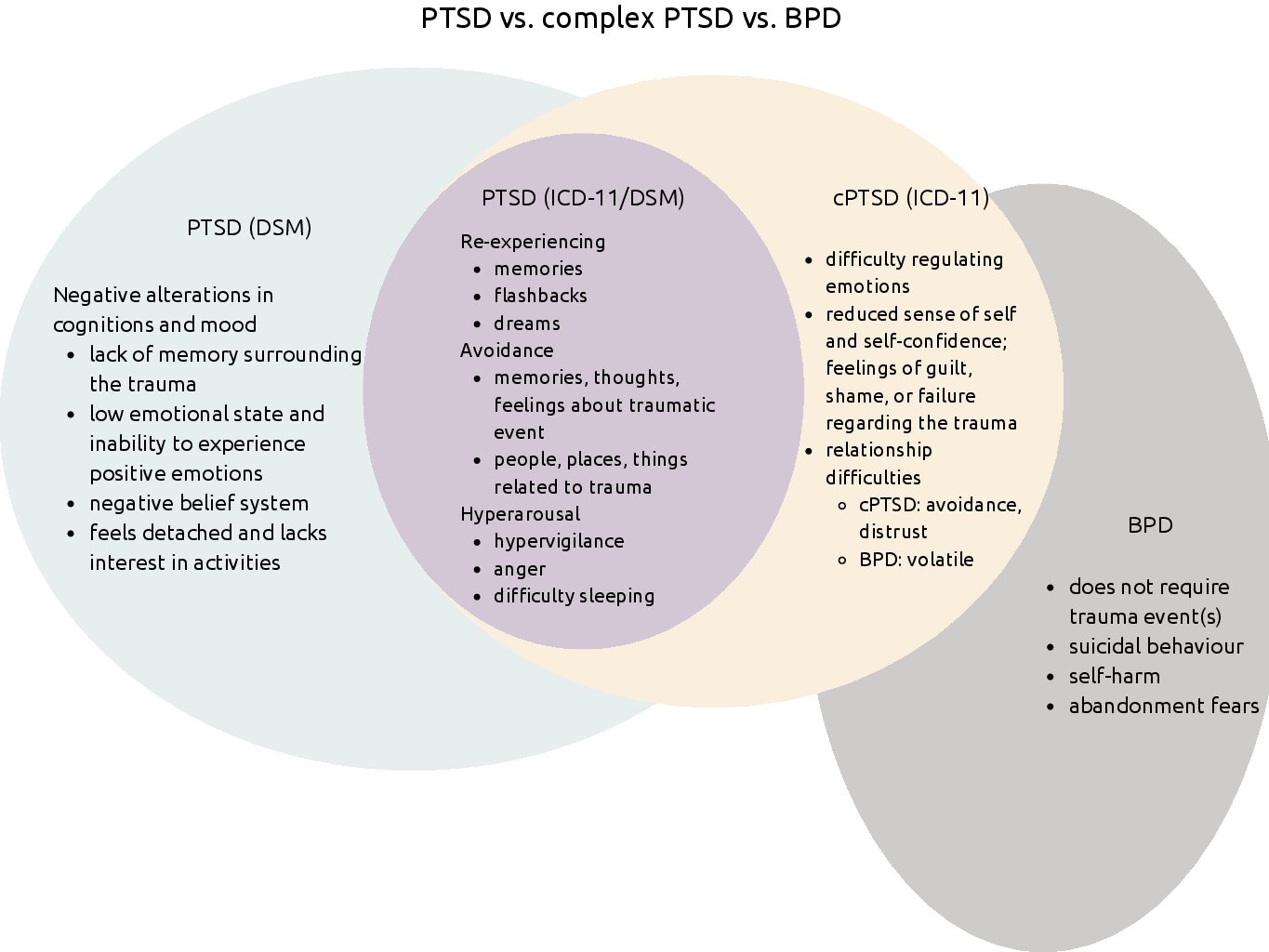
Both the DSM-5-TR and ICD-11 include the PTSD diagnosis and both require a traumatic event to have occurred (this becomes important when we look at BPD). Until the recent DSM revision, both reference manuals looked at PTSD criteria as a three factor model. The three categories of symptoms are ‘re-experiencing’, ‘avoidance’, and ‘hyperarousal’. The DSM-5-TR has altered the cluster of symptoms identified as avoidance into ‘avoidance’ and a new category, ‘negative alterations in cognitions and mood.’
Why the long explanation regarding the DSM-5-TR and the ICD-11? This is where they differ in the context of trauma diagnoses pertaining to this article. The DSM does not have a complex PTSD (cPTSD) diagnosis but the ICD-11 does. The diagnostic criteria for cPTSD includes the criteria for PTSD as well as the following disturbances in self-organization; difficulties with emotion regulation, reduced self-confidence along with feelings of guilt, shame, or failure regarding the trauma, and relationship difficulties.
The diagnostic criteria for PTSD requires the exposure to a traumatic event, however cPTSD typically involves ongoing, repeated trauma that often occurred in childhood and this abuse was usually by a caregiver or someone seen as an authority figure such as a priest or a teacher. The trauma could have been physical, emotional, or sexual abuse.
Now that we have a better understanding of current guidelines for PTSD and cPTSD, let’s look at BPD. Complex PTSD and BPD are mostly separate diagnoses except for the overlap in affective dysregulation. This includes the following:
- Unstable, intense relationships
- Unstable affect
- Lack of self-awareness
However, these three symptoms look differently depending on if we’re considering cPTSD or BPD. With cPTSD difficult relationships are a result of distrust and avoidance where as one with BPD often has difficulty with relationships due to volatility. BPD also prompts abandonment fears and an unstable sense of self compared to cPTSD often indicating a consistent negative sense of self. As far as emotion regulation, cPTSD includes emotional sensitivity, reactive anger, and poor coping. People with BPD may exhibit some of the same, but more typically struggle with thoughts of suicidality and self-harm which occurs less frequently with cPTSD.
Lastly, what about trauma and BPD? Although PTSD and BPD are often seen together, a diagnosis of BPD does not require a traumatic event to have occurred.
Ready to start the recovery process from trauma and/or BPD? I use an effective combination of psychodynamic/Adlerian and dialectical behaviour therapy (DBT). Book your complimentary session today!
References:
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596
Bongaerts, H., Voorendonk, E.M., Van Minnen, A., Rozendaal, L., Telkamp, B.S.D., & de Jongh, A. (2022). Fully remote intensive trauma-focused treatment for PTSD and complex PTSD. European Journal of Psychotraumatology, 13(2), 1-13. https://doi.org/10.1080/20008066.2022.2103287
Cloitre, M., Garvert, D.W., Weiss, B., Carlson, E.B., & Bryant, R.A. (2014). Distinguishing PTSD, complex PTSD, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology, 5. https://doi.org/10.3402/ejpt.v5.25097
Franco, F. (2021). Understanding and treating C-PTSD. Journal of Health Service Psychology, 47, 85-93. https://doi.org/10.1007/s42843-021-00038-1
Jowett, S., Karatzias, T., Shevlin, M., & Albert, I. (2020). Differentiating symptom profiles of ICD-11 PTSD, complex PTSD, and borderline personality disorder: A latent class analysis in a multiply traumatized sample. Personality Disorders: Theory, Research, and Treatment, 11, 36-45. https://doi.org/10.1037/per0000346
Kira, I.A., Shuwiekh, H. & Laddis, A. (2023). The linear and non-linear association between trauma dissociation, complex PTSD, and executive function deficits: A longitudinal structural equation modeling study. Journal of Loss and Trauma, 28(3), 217-234. https://doi.org/10.1080/15325024.2022.2101734
Owczarek, M., Karatzias, T., McElroy, E., Hyland, P., Cloitre, M. Kratzer, L. Knefel, M., Grandison, G., Ho, G.W.K., Morris, D., & Shevlin, M. (2023). Borderline personality disorder (BPD) and complex posttraumatic stress disorder (CPTSD): A network analysis in a highly traumatized clinical sample. Journal of Personality Disorders, 37(1), 112-129. https://doi.org/10.1521/pedi.2023.37.1.112
World Health Organization. (2023). International Statistical Classification of Diseases and Related Health Problems (11th ed.). https://icd.who.int/

0 Comments